July 2019
Ankle Pain
Ankle pain can often occur due to a number of conditions including ankle fracture, arthritis, instability, tendonitis, and gout. Symptoms that accompany ankle pain may include swelling, stiffness, redness, and warmth in the affected area. Pain associated with the ankle is typically described as a dull and intense ache that is felt during ankle motion or when bearing weight.
While ankle pain treatment can vary depending on what the condition is and how severe it is, initial treatment often involves rest, ice, elevation, and immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may also be prescribed. Other possible treatments include physical therapy and cortisone injection. Your podiatrist can determine the method of treatment that is most appropriate for you and your condition.
Causes of Ankle Pain and Treatment Options
There can be many diffe rent causes of ankle pain, ranging from an ankle sprain or fracture to chronic conditions such as arthritis. The degree of the ankle pain can vary and it can come on suddenly or slowly over time. The ankle joint consists of bones, muscles, cartilage, and tissues called ligaments and tendons. Any injury or disease that were to affect these structures, could very well lead to ankle pain. Some causes of ankle pain include sprains, tendonitis, arthritis and a bruise or break of the bone. It is important to know that you should visit a doctor if there is an inability to bend the ankle, swelling of the joint, signs of an infection, an inability to walk comfortably on the affected side and if you have ankle pain that occurs at night or while resting. Ankle pain can be diagnosed with an X-ray, medical exam or thorough physical examination. The RICE protocol is a 4-step process in which you may be able to treat your injury from the comfort of your own home. The first step is to rest. This will allow for the joint to relax and for any inflammation to subside. The next step is to ice. Ice should be applied at least 3 times a day for 15 to 20 minutes. This will allow for any swelling to go down and it will also soothe the pain. The third step is to add compression. Compression bandages, such as an ACE wrap will help support and immobilize the ankle joint. Be sure not to add too much compression as this can lead to numbness, tingling and swelling at the site of the pain. The final step is to elevate the ankle. Raising the ankle above the level of the heart, by way of propping your foot up on pillows, will help reduce any swelling for the first couple days after the injury has occurred. If you are suffering from any ankle pain, visit your podiatrist to see what treatment may be right for you.
rent causes of ankle pain, ranging from an ankle sprain or fracture to chronic conditions such as arthritis. The degree of the ankle pain can vary and it can come on suddenly or slowly over time. The ankle joint consists of bones, muscles, cartilage, and tissues called ligaments and tendons. Any injury or disease that were to affect these structures, could very well lead to ankle pain. Some causes of ankle pain include sprains, tendonitis, arthritis and a bruise or break of the bone. It is important to know that you should visit a doctor if there is an inability to bend the ankle, swelling of the joint, signs of an infection, an inability to walk comfortably on the affected side and if you have ankle pain that occurs at night or while resting. Ankle pain can be diagnosed with an X-ray, medical exam or thorough physical examination. The RICE protocol is a 4-step process in which you may be able to treat your injury from the comfort of your own home. The first step is to rest. This will allow for the joint to relax and for any inflammation to subside. The next step is to ice. Ice should be applied at least 3 times a day for 15 to 20 minutes. This will allow for any swelling to go down and it will also soothe the pain. The third step is to add compression. Compression bandages, such as an ACE wrap will help support and immobilize the ankle joint. Be sure not to add too much compression as this can lead to numbness, tingling and swelling at the site of the pain. The final step is to elevate the ankle. Raising the ankle above the level of the heart, by way of propping your foot up on pillows, will help reduce any swelling for the first couple days after the injury has occurred. If you are suffering from any ankle pain, visit your podiatrist to see what treatment may be right for you.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
An Overview of Flat Feet
Flat feet is a deformity that occurs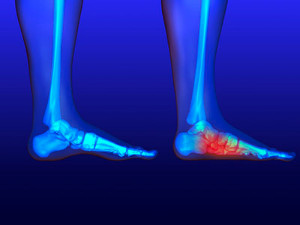 when the arch of the foot collapses and comes into complete or near-complete contact with the ground. The condition occurs either at the time of birth or through injury and age. For the people that do develop flat feet, there are very few symptoms. They can include a limited range of motion, swelling along the inner ankle and arch of the foot, and unbearable pain when standing on your feet. The main cause of flat feet is excessive pronation of the foot. This means that the arch descends downward and inward as the foot strikes the ground. Due to the tendency for flat feet to over pronate, they are less able to absorb shock, placing persistent stress on the feet, ankles, and knees. If the inward tilt of the foot places further strain on the tendons and ligaments of the lower extremities, this can also result in Achilles tendinitis and chronic knee pain. Flat feet is most common in newborns and toddlers due to the arches on their feet not having developed yet. Imaging tests done to determine if someone has flat feet are X-rays, ultrasounds and MRIs. The treatments vary for children and adults. The most beneficial treatment for children would be walking barefoot during developmental years. For adults, the best forms of treatment are exercises that increase arch flexibility and strength such as foot gymnastics, a runner’s stretch, the yoga pose downward dog and therapeutic massages. If you feel you are developing flat feet, it is recommended to see a podiatrist so they can provide the best treatment option.
when the arch of the foot collapses and comes into complete or near-complete contact with the ground. The condition occurs either at the time of birth or through injury and age. For the people that do develop flat feet, there are very few symptoms. They can include a limited range of motion, swelling along the inner ankle and arch of the foot, and unbearable pain when standing on your feet. The main cause of flat feet is excessive pronation of the foot. This means that the arch descends downward and inward as the foot strikes the ground. Due to the tendency for flat feet to over pronate, they are less able to absorb shock, placing persistent stress on the feet, ankles, and knees. If the inward tilt of the foot places further strain on the tendons and ligaments of the lower extremities, this can also result in Achilles tendinitis and chronic knee pain. Flat feet is most common in newborns and toddlers due to the arches on their feet not having developed yet. Imaging tests done to determine if someone has flat feet are X-rays, ultrasounds and MRIs. The treatments vary for children and adults. The most beneficial treatment for children would be walking barefoot during developmental years. For adults, the best forms of treatment are exercises that increase arch flexibility and strength such as foot gymnastics, a runner’s stretch, the yoga pose downward dog and therapeutic massages. If you feel you are developing flat feet, it is recommended to see a podiatrist so they can provide the best treatment option.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Robert Graser from Graser Podiatry and Bunion Surgery Institute. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Boerne, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flip Flops and Your Feet
When the weather heats up, you may want to start wearing flip-flops. However, it has been proven that these are not the ideal shoes in terms of preserving the health of your feet.
Flip flops are known to expose your feet to different types of bacteria and fungal infections. When you wear your flip flops in public, you are exposing them to staphylococcus which is a skin-irritating bacterium. Athlete’s foot is also highly contagious and can be spread when you walk around nearly-barefoot.
Another harmful effect of wearing flip-flops is that they develop blisters on the feet. This is because the thin strap rubs against the skin with each step taken. Unfortunately, when blisters pop, they cause you to be more vulnerable to pathogens you pick up by having your feet exposed.
These shoes may also cause “shooting pains”. If you have flat feet, you need arch support to keep your knees, hips, and back in alignment. If you wear flat shoes, your joints are forced to compensate which can cause injuries throughout the body.
If you constantly wear flip-flops, you should avoid doing so as they can lead to many problems for your feet. If you are experiencing any of these foot issues, you should seek help from a podiatrist right away.
Woes for Your Toes from Flip-Flops
Flip-flops are fun to wear wh en lounging out by the pool or when going to the beach. At the same time, they could be causing major stress and injury to the feet. Without any protective outer covering on your flip-flops, it can be easy for the feet to get cut or bruised. Also, due to the feet not being protected by socks in flip-flops, the skin on the feet is more prone to sunburn, as well as blisters from rubbing against the thong of the flip-flop. Flip-flops may seem easier to slip on than shoes, but this isn’t actually the case. The feet work a lot harder in order to keep the flip-flops on. This causes the toes to involuntarily curl up and the muscles on the feet to strain which can lead to bunions or hammertoes. In addition, the base of the flip-flop that is meant to support the foot isn’t doing that at all and instead is overworking the foot’s tendons and ligaments. This can cause overuse injuries such as shin splints, tendonitis and plantar fasciitis. Activities that aren’t meant to be done in flip-flops include hiking, biking, working with tools and sporting activities. Consult a podiatrist to get a better idea of when you should wear flip-flops.
en lounging out by the pool or when going to the beach. At the same time, they could be causing major stress and injury to the feet. Without any protective outer covering on your flip-flops, it can be easy for the feet to get cut or bruised. Also, due to the feet not being protected by socks in flip-flops, the skin on the feet is more prone to sunburn, as well as blisters from rubbing against the thong of the flip-flop. Flip-flops may seem easier to slip on than shoes, but this isn’t actually the case. The feet work a lot harder in order to keep the flip-flops on. This causes the toes to involuntarily curl up and the muscles on the feet to strain which can lead to bunions or hammertoes. In addition, the base of the flip-flop that is meant to support the foot isn’t doing that at all and instead is overworking the foot’s tendons and ligaments. This can cause overuse injuries such as shin splints, tendonitis and plantar fasciitis. Activities that aren’t meant to be done in flip-flops include hiking, biking, working with tools and sporting activities. Consult a podiatrist to get a better idea of when you should wear flip-flops.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact Dr. Robert Graser from Graser Podiatry and Bunion Surgery Institute. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions please feel free to contact our office located in Boerne, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
What Is Tarsal Tunnel Syndrome?
 The tarsal tunnel is a narrow space that is on the inside of the ankle next to the ankle bones. It is covered with a thick ligament that protects structures within the tunnel such as arteries, veins, tendons and nerves. Tarsal tunnel syndrome is a compression or squeezing on the posterior tibial nerve that produces symptoms from the inside of the foot into the ankle. Some symptoms of tarsal tunnel syndrome include numbness, a shooting pain, and tingling or burning sensations that are similar to an electric shock. Some causes are diabetes which can cause swelling on the nerve, an injury like an ankle sprain that can produce swelling in or near the tunnel, and flat feet due to the outward tilting of the heel. It is important to go see your local podiatrist if you feel you exhibit any of these symptoms.
The tarsal tunnel is a narrow space that is on the inside of the ankle next to the ankle bones. It is covered with a thick ligament that protects structures within the tunnel such as arteries, veins, tendons and nerves. Tarsal tunnel syndrome is a compression or squeezing on the posterior tibial nerve that produces symptoms from the inside of the foot into the ankle. Some symptoms of tarsal tunnel syndrome include numbness, a shooting pain, and tingling or burning sensations that are similar to an electric shock. Some causes are diabetes which can cause swelling on the nerve, an injury like an ankle sprain that can produce swelling in or near the tunnel, and flat feet due to the outward tilting of the heel. It is important to go see your local podiatrist if you feel you exhibit any of these symptoms.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Dr. Robert Graser of Graser Podiatry and Bunion Surgery Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Boerne, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
Featured Articles
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018